Vivo Pathophysiology
The Parietal Cell: Mechanism of Acid Secretion
The best-known component of gastric juice is hydrochloric acid, the secretory product of the parietal, or oxyntic cell. It is known that the capacity of the stomach to secrete HCl is almost linearly related to parietal cell numbers.
When stimulated, parietal cells secrete HCl at a concentration of roughly 160 mM (equivalent to a pH of 0.8). The acid is secreted into large cannaliculi, deep invaginations of the plasma membrane which are continuous with the lumen of the stomach.
When acid secretion is stimulated there is a dramatic change in the morphology of the membranes of the parietal cell. Cytoplasmic tubulovesicular membranes which are abundant in the resting cell virtually disappear in concert with a large increase in the cannalicular membrane. It appears that the proton pump as well as potassium and chloride conductance channels initially reside on intracellular membranes and are transported to and fused into the cannalicular membrane just prior to acid secretion.
The epithelium of the stomach is intrinsically resistant to the damaging effects of gastric acid and other insults. Nonetheless, excessive secretion of gastric acid is a major problem in human and, to a lesser extent, animal populations, leading to gastritis, gastric ulcers and peptic acid disease. As a consequence, the parietal cell and the mechanisms it uses to secrete acid have been studied extensively, leading to development of several drugs useful for suppressing acid secretion.
Mechanism of Acid Secretion
The hydrogen ion concentration in parietal cell secretions is roughly 3 million fold higher than in blood, and chloride is secreted against both a concentration and electric gradient. Thus, the ability of the partietal cell to secrete acid is dependent on active transport.
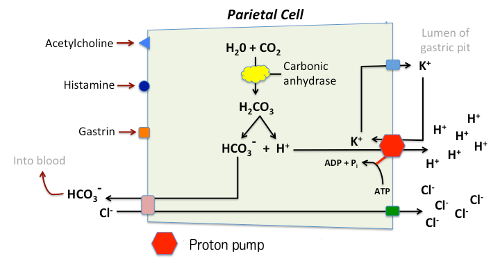
The key player in acid secretion is a H+/K+ ATPase or "proton pump" located in the cannalicular membrane. This ATPase is magnesium-dependent, and not inhibitable by ouabain. The current model for explaining acid secretion is as follows:
- Hydrogen ions are generated within the parietal cell from dissociation of water. The hydroxyl ions formed in this process rapidly combine with carbon dioxide to form bicarbonate ion, a reaction cataylzed by carbonic anhydrase.
- Bicarbonate is transported out of the basolateral membrane in exchange for chloride. The outflow of bicarbonate into blood results in a slight elevation of blood pH known as the "alkaline tide". This process serves to maintain intracellular pH in the parietal cell.
- Chloride and potassium ions are transported into the lumen of the cannaliculus by conductance channels, and such is necessary for secretion of acid.
- Hydrogen ion is pumped out of the cell, into the lumen, in exchange for potassium through the action of the proton pump; potassium is thus effectively recycled.
- Accumulation of osmotically-active hydrogen ion in the cannaliculus generates an osmotic gradient across the membrane that results in outward diffusion of water - the resulting gastric juice is 155 mM HCl and 15 mM KCl with a small amount of NaCl.

A key substrate in the production of gastric acid is CO2, and diffusion of CO2 through the basal surface of the parietal appears to be the rate limiting step in acid synthesis. Interestingly, this biochemical principle has been validated by studying gastric function in alligators. These reptiles produce huge amounts of gastric acid after ingestion of a large carcass, and abundant acid seems to be important in speeding digestion of bone. Alligators have a vascular shunt that diverts CO2-rich venous blood to the stomach rather than directly back to the lungs, increasing the amount of CO2 that diffuses into parietal cells and thereby enhancing synthesis of acid.
Control of Acid Secretion
Parietal cells bear receptors for three stimulators of acid secretion, reflecting a triumverate of neural, paracrine and endocrine control:
- Acetylcholine (muscarinic type receptor)
- Gastrin
- Histamine (H2 type receptor)
Histamine from enterochromaffin-like cells may well be the primary modulator, but the magnitude of the stimulus appears to result from a complex additive or multiplicative interaction of signals of each type. For example, the low amounts of histamine released constantly from mast cells in the gastric mucosa only weakly stimulate acid secretion, and similarly for low levels of gastrin or acetylcholine. However, when low levels of each are present, acid secretion is strongly forced. Additionally, pharmacologic antagonists of each of these molecules can block acid secretion.
Histamine's effect on the parietal cell is to activate adenylate cyclase, leading to elevation of intracellular cyclic AMP concentrations and activation of protein kinase A (PKA). One effect of PKA activation is phosphorylation of cytoskeletal proteins involved in transport of the H+/K+ ATPase from cytoplasm to plasma membrane. Binding of acetylcholine and gastrin both result in elevation of intracellular calcium concentrations.
Several additional mediators have been shown to result in gastric acid secretion when infused into animals and people, including calcium, enkephalin and bombesin. Calcium and bombesin both simulate gastrin release, while opiate receptors have been identified on parietal cells. It is unclear whether these molecules have a significant physiologic role in parietal cell function.
A variety of substances are capable of reducing gastric acid secretion when infused intravenously, including prostaglandin E2 and several peptides hormones, including secretin, gastric inhibitory peptide, glucagon and somatostatin. PGE2, secretin and somatostatin may be physiologic regulators. Somatostatin inhibits secretion of gastrin and histamine, and appears to have a direct inhibitory effect on the parietal cell.
References and Reviews
- Farmer CG, Uriona TJ, Olsen DB, Steenblik M, Sanders K. The right-to-left shunt of crocodilians serves digestion. Physiol Biochem Zool 2008; 81:125-137.
- Forte JG, Zhu L. Apical Recycling of the Gastric Parietal Cell H,K-ATPase. Annu Rev Physiol 72:273–96, 2010
- Kidder GW, Montgomery CW. CO2 diffusion into frog gastric mucosa as rate-limiting factor in acid secretion. Am J Physiol 1974; 227:300–304.
- Samuelson LC, Hinkle KL: Insights into the regulation of gastric acid secretion through analysis of genetically engineered mice. Annu Rev Physiol 65:383-400, 2003.
- Yao X, Forte JG: Cell biology of acid secretion by the parietal cell. Annu Rev Physiol 65:103-131, 2003.
Send comments to Richard.Bowen@colostate.edu
A Bosnian translation of this page by Amina Dugalic is available at Bosnian translation
A Ukrainian translation of this page by Olena Chervona is available at Ukrainian translation
